Deliver lasting relief for patients with gut-brain conditions like IBS – no restrictions or waitlists for them, no extra work for you.
Refer a patientRequest clinician access



















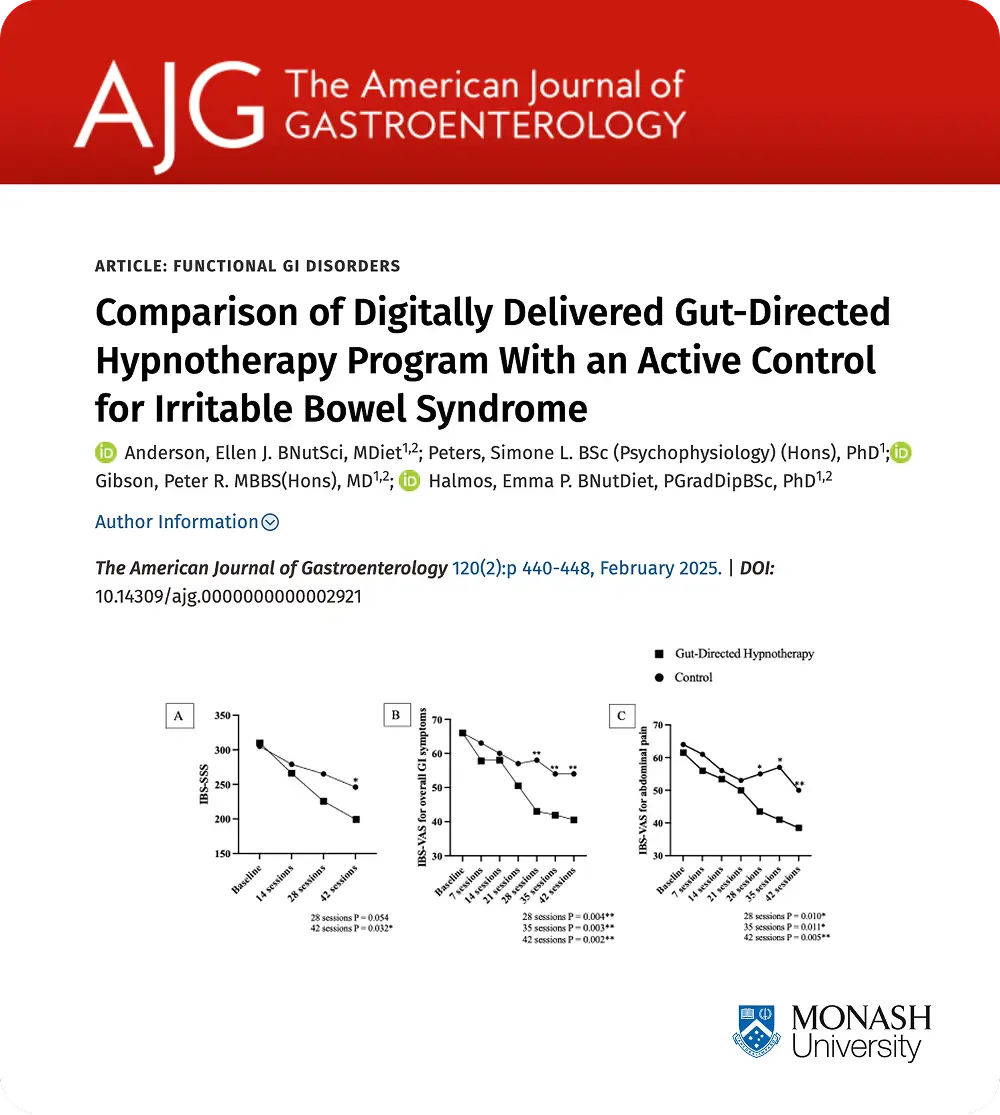
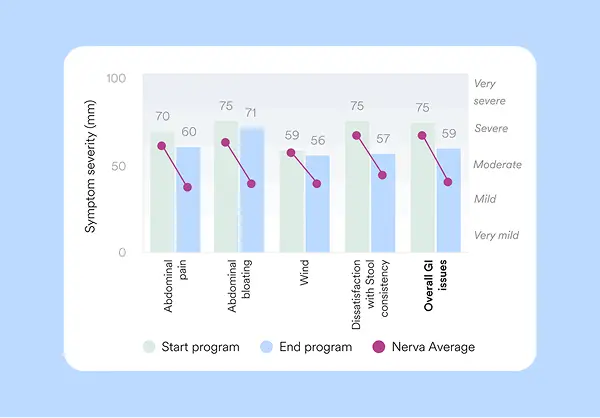
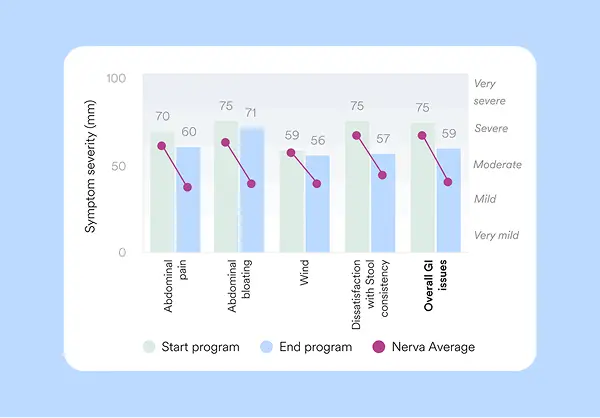
Nerva’s efficacy and safety has been demonstrated across 5 published clinical studies, including a large peer-reviewed randomized controlled trial¹, showing that Nerva:




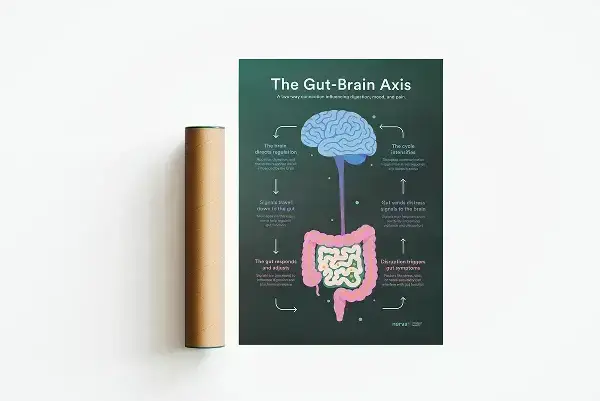
Nerva helps you provide multidisciplinary care by delivering gut-brain therapy virtually – supporting patients with gut-brain disorders like IBS by helping them retrain how the brain and gut communicate.

Nerva has demonstrated efficacy across all IBS subtypes and a broad range of patient profiles. It may be particularly appropriate for individuals who:

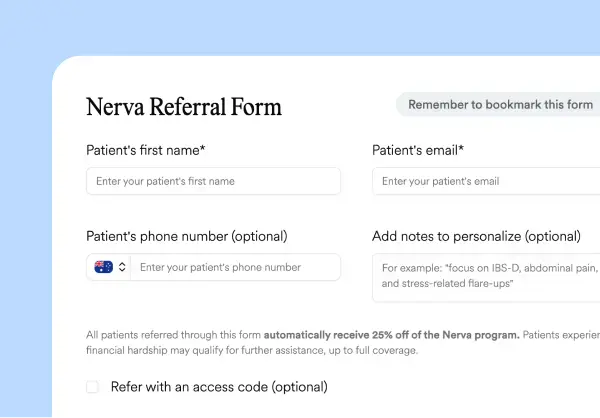
Nerva supports accessibility by reducing financial barriers to care. All patients referred through Nerva’s HIPAA-compliant referral form automatically receive a 25% referral adjustment, reducing the annual subscription cost to $149.25 USD. If cost remains a concern, patients may be eligible for additional support through Nerva’s Patient Assistance Program.



Enhance your next gut-brain disorder consult with complimentary physical resources developed by Nerva’s clinical specialists.


Send an inquiry or book a brief call with our clinical team to discuss Nerva, referral options, EMR integration, or to organize a lunch and learn for your clinic.



Nerva is offered as an annual subscription. Patients referred through the clinician form automatically receive 25% off, bringing the cost down to $149.25 USD. While Nerva isn’t currently covered by insurance, the cost is comparable to a single GI psychology session and includes 12 months of access. Patients experiencing financial hardship may be eligible for full or partial coverage through Nerva’s Patient Assistance Program.
Patients begin with a 7-day free trial to explore the program risk-free. For added peace of mind, we also offer a 42-day money-back guarantee.
Nerva builds off the Monash University gut-directed hypnotherapy protocol and is validated in multiple published clinical studies. In a randomized controlled trial, 81% of participants achieved significant symptom improvement¹. Research from Monash University also found that gut-directed hypnotherapy works just as well as the low FODMAP diet for managing IBS symptoms². Nerva was co-founded by Dr. Simone Peters, one of the lead researchers on this study. Nerva’s efficacy has been demonstrated across all IBS subtypes, with improvements shown to be sustained long-term.
Explore more research.
Explain it as a form of gut-brain therapy that helps retrain communication between the brain and digestive system. It uses guided relaxation and visualization to reduce the brain’s sensitivity to gut signals – similar to calming an overactive alarm system. You can describe it as a clinically validated practice that helps patients manage symptoms by addressing the underlying gut-brain connection.
To learn more about how Nerva works, see our Mechanism of Action section.
Referrals can be made in seconds through Nerva’s secure online form. Once referred, Nerva handles onboarding, follow-up, and support.
Clinicians receive progress updates with symptom tracking (IBS-SSS and PHQ-4) through our HIPAA-compliant reporting system.
Nerva is designed to be seamlessly integrated into clinical practice. Referrals take less than 30 seconds, and the Nerva team manages patient communication and support. It complements existing dietary, pharmacologic, or psychological interventions without adding administrative burden. Nerva can be incorporated into a patient’s care plan at any stage of treatment.
Nerva meets HIPAA and SOC 2 compliance standards. All patient data is encrypted in transit and at rest, and never shared without consent. Clinicians can refer and track patients confidently knowing Nerva meets the highest data privacy and security standards.
Nerva is not a medical treatment or diagnostic device. It is a self-guided program designed to support people with diagnosed Irritable Bowel Syndrome (IBS) or other disorders of gut-brain interaction (DGBI) managing their symptoms and improving quality of life.
1) Anderson, Ellen J. BNutSci, MDiet1,2; Peters, Simone L. BSc (Psychophysiology) (Hons), PhD1; Gibson, Peter R. MBBS(Hons), MD1,2; Halmos, Emma P. BNutDiet, PGradDipBSc, PhD1,2. Comparison of Digitally Delivered Gut-Directed Hypnotherapy Program With an Active Control for Irritable Bowel Syndrome. The American Journal of Gastroenterology 120(2):p 440-448, February 2025. | DOI: 10.14309/ajg.0000000000002921 2) Peters, S. L., Yao, C. K., Philpott, H., Yelland, G. W., Muir, J. G., & Gibson, P. R. (2016). Randomised clinical trial: the efficacy of gut-directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome. Alimentary pharmacology & therapeutics, 44(5), 447–459. https://doi.org/10.1111/apt.13706